Cancer struck Sonya Van Dam, the wife of wrestler Rob Van Dam, out of the blue and challenged the couple in unexpected ways. In an exclusive, two-part interview with SLAM! Wrestling, Sonya and Rob document their journey with overcoming colon cancer and in the process, reveal some of the checks and balances — or lack thereof — of the American health care system.
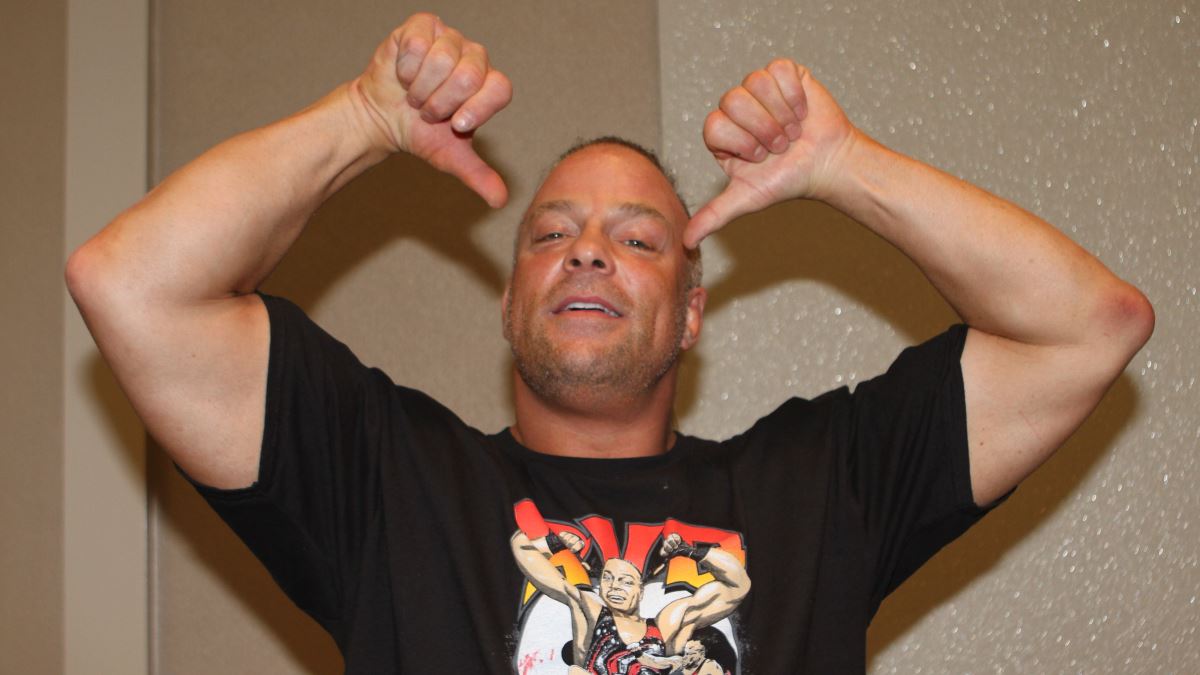
Rob and Sonya Van Dam. Photos all courtesy the Van Dams.
This was an understandably difficult subject for Sonya to lay bare and it took several months for her to mentally prepare for the discussion. Their journey started in February in 2007 and is nearing its fruition here in the summer of 2009. We start, naturally, from the beginning.
It was February of 2007, when an unusual bout of stabbing stomach pain combined with ineffective prescription fibre pills left Sonya Van Dam searching for answers. Her body was trying to tell her something. Though it was indirectly all around her, colon cancer was something that was the farthest thing on her mind. “I had no idea. I honestly thought it could have been irritable bowel syndrome, that’s why I ate the fibre pills for so long and wanted to believe that they worked,” she said. “Of course I thought initially, ‘Oh, this could be cancer.’ But it wasn’t a serious thought; it was just one of those ‘Oh, I just checked my symptoms on the internet, I’m going to be fine.’
“My friend Tina Mucciolo [Louie Spicolli’s sister], her mother passed away from cancer. But that was six months after Louie died, and that was before we moved here, so I really dealt with the after-effect of the grief that Tina went through,” she recalled. “But I’ve never had cancer touch my life like this. My adopted grandfather died of liver cancer, but we didn’t know that until after he was dead. We didn’t know. He didn’t go through chemo or anything. They’re secretive like that. You didn’t talk about cancer in their generation. It was the c-word and you whispered about it. I didn’t know until two years after he died that he died of liver cancer. He was 89 years old.”
Rob Van Dam’s experience was similar. “Cancer was something that I heard about, but it didn’t affect me at all, it was something that just happened to other people,” he admitted. “But now that we’re past this, and everybody is aware of our situation, I find that it is was way more common than I ever realized. I seems that almost everyone that I know has been affected by cancer either from a family member, a loved one, or someone very close to them. From doing some studying, I’ve learned that 1-in-2 men and 1-in-3 women can get cancer, so the odds are incredibly high that somebody, if they don’t know somebody that’s gone through this, they probably will.”
On the horizon was a show for RVD in Portugal, just a week away. It was the perfect getaway, an opportunity to soak up the sights and sounds of the country. But the stomach pains were an issue, and through a neighbor’s recommendation, Sonya sought a second opinion from Dr. Sitaraman Jyotheeswaran, the physician she affectionately referred to as Dr. J. “He is a phenomenal doctor,” she gushed. “He was educated in England, he’s from India and I honestly believe because he is an outside-of-the-box thinker, that’s why he gave a 32-year-old woman a colonoscopy. None of the other doctors wanted to do it, because I don’t have a family history of colorectal cancer. So nobody wanted to do it.”
“The blood in the stool should have been the first sign. My [first] doctor missed that entirely. He thought it was either a hemorrhoid or irritable bowel syndrome.”
Sonya heard through a neighbour that her case shocked Dr. J’s staff to the point where they all had personal colonoscopies done, but she had seen several doctors before him.
“I went to the ER and that doctor blew me off and wrote a prescription for Xantax, which is an over-the-counter indigestion medication. That’s the equivalent of someone coming in with part of their brain bleeding and then giving them some Tylenol. And the medical system here in California is different. I’ve lived all over the country, five different states and California has a very strange medical system. We have a lot of tiny little hospitals, not one big hospital.
“We live along the coast, by Long Beach. On the east coast, they usually have one big university hospital or two major hospitals for the city. Los Angeles is not like that; we have tiny neighborhood hospitals spread along the city.
Sonya Van Dam.
“If you get in a serious accident, and you’re on the wrong side of town, if you’re in serious trauma, you could possibly die, because they can’t get you to the right hospital. It’s just not equipped to deal with major traumas. It’s very bizarre; it’s like a dirty little secret here in Los Angeles.”
Sonya had the colonoscopy when she came back from Portugal, unprepared for the salty lemonade she ingested to ‘prep,’ which would induce what she gracefully described as “violent diarrhea.”
She was even more unprepared for the result.
“At that moment, you just go numb,” she said vividly. “The feeling where I can describe it as I didn’t hear the other words that were coming out of his mouth. It was almost like a movie. Every time I’ve seen that in movies I was like, ‘Oh, whatever. Talk about dramatic.’ No, it really happens like, his lips were moving, I was not hearing anything else coming out of his mouth. Because all I could hear in my head was, ‘Did he just say I have cancer? No way. He just said I didn’t have cancer.’ And that’s all I can say, and my head is nodding and I’m agreeing with everything but have no idea what he is saying.
“It didn’t really dawn on me until the doctor gets up and leaves, and I have no idea what he said other than what I’m processing in my brain as, ‘You don’t have cancer.’
“So the nurse comes in and she’s helping me get into the wheelchair because now I’m getting wheeled to the parking lot and she wheels me out, and her and then the other two nurses that were working in the recovery room both rush over and they’re like, ‘I’m so sorry, sweetie, you didn’t get the results you were looking for today. You’ve got a really long hard road ahead of you, but you’re young, you’re going to do fine.’ And in that exact moment, I was like ‘Holy s—, I have cancer; he said I had cancer.'”
“That’s when it really sunk in for me that I had cancer, was when those nurses were like ‘Sweetie, I’m so sorry.'”
“We were actually still in the doctor’s office just moments after hearing the news, we were still kind of in shock, and didn’t really know how to react,” concurred Rob. “I mean I didn’t want her to know that I was freaking out; I wanted to be strong for her. Just literally seconds afterwards, she turned to me and said, ‘We have to tell everybody; if it can happen to me, it can happen to them.'”
That led to her revealing the news on her MySpace page.
Sonya elaborated on the moment. “I dealt with it very matter-of-factly. At this point, I have to call my family and tell them I have colon cancer, which is not the easiest thing. It surprised me how I dealt with it, honestly. It shocked me that I was so matter-of-fact about it. You really don’t know how you’re going to react until something like that happens.
“I always expected that I would fall part, or I would just be a sobering mess, my-life-is-over type of thing. I guess I manned up. I took it, I didn’t cry. It freaked me out that I didn’t cry for a long time until like right before my surgery. I found out April 5, [2008] that I had cancer. My surgery was April 25, so I didn’t have a lot of time to process.
“Everything was so fast, because between that time you have to 1: process and accept that you have cancer; 2: shop for a surgeon, which can I just tell you, is the strangest thing I’ve ever had to shop for in my life. I love shoes, but it’s very surreal to shop for a surgeon. And they all have egos the size of California.”
The doctor-searching process seemed rather impersonal to her at first.
“What I didn’t like was that there was no real support system,” she observed. “If I had gone with one of my local surgeons, they just sent me to the local oncologist and it’s just kind of like you’re on your own. There’s no team that works on you or for you. I felt like I needed more, like this was so much bigger than me. I didn’t understand everything that was happening to me and so my neighbor suggested I go to City of Hope.”
The City of Hope.
According to its website, City of Hope is a non-for-profit organization and one of only 40 National Cancer Institute (NCI) certified centers in the United States. Supported by various fundraisers, public and corporate contributions and established in 1913, it is nearing 100 years in existence. One of their core mandates is to research and develop an active cure for cancer.
The centre answers the question of why people should use their services: “At City of Hope, we treat people who have cancer and other serious illnesses, not simply the symptoms and the disease. We strive to treat the whole patient, and we do it with respect, honor, humanity and understanding.”
Famed musician Sheryl Crow has recorded various public service announcements for the City of Hope.
“I went and interviewed the surgeons there, and I had a great feeling,” Sonya explained. “The first thing they said was, ‘When you’re a patient here at City of Hope, you’re a patient for life. We don’t let you go. You’re always in our databanks; if some new treatment comes in and it affects you — because that’s the cancer you have — we’re going to call you. We’re going to make you know that this treatment is here and available for you.’ So right off the bat, this is what I was looking for.
“They have a team of doctors. I have one primary doctor that I see, but that primary doctor every week has case meetings with six other doctors. So six other doctors are going through my chart and my case and discussing every treatment protocol that they put me on. So that felt a lot better. And being 32, this is the other thing. I’m a 32-year-old woman with colon cancer; it is as odd as you can get.
“Colon cancer is my grandpa’s disease. It’s primarily men and primarily men over 50,” she continued. “So for a 32-year-old woman to have it was just bizarre, and my local surgeons and doctors were acting like, ‘Oh, we see this every day,’ which I knew they didn’t. And for them to act like they did, it was almost felt like they were belittling it, and I didn’t like that either. When I went to City of Hope, it was like, ‘This is bizarre. You are a very special case. We want to study you,’ which never feels good to hear that they want you to be a lab rat, but at the same time, it feels great to know that someone feels your cancer is as strange as you do, and they want to get to the bottom of it.”
“My surgeon and my life-saving doctor was Dr. Benjamin Paz. He saved my life, because on April 25, 2008, I went into surgery, and they removed half of my colon. They were just going to take the section that had the tumor in it, because at this point, I’ve not been staged. I can’t get staged until they take the tumor out. So they go in and they take out my entire ascending colon, and half of my transverse and 35 lymph nodes, which was a lot more than they expected to take out. The tumor was a lot larger than they expected. It was 6.6 cm in diameter. Three of the lymph nodes were infected, which meant stage three. There are only four stages of cancer. Stage five is death. And here I am at stage three.
“The surgery was brutal, because first the colon is missing and all you eat is ice chips. I wasn’t hungry, but I wanted to eat something badly,” she laughed.
“I was out of the hospital after five days, after the surgery and I have to wait two weeks for the staging [a determination of how advanced the cancer is], which is its own form of torture because if I’m stage one or two, I don’t have to have chemotherapy. Rob’s like, ‘Oh, you’re stage one. I can feel it, you’re stage one.’ I knew by the pain was in that I was further along than stage one, but I wasn’t willing to say stage three, so I figured stage two. We actually had bets before the doctor came in to see what stage I was in because you have to laugh, or you’re going to go insane,” she explained.
“So we’re making bets, and Dr. Paz, he has a great sense of humour and he’s always smiling. He wasn’t smiling when he came in, and I knew right away something was wrong. He said, ‘It kind of us by surprise, no one was expecting your tumor to be as far advanced as it was.’ I’m like, ‘Just tell me.’ He said, ‘I’m sorry, but it’s stage three.’ I’m like, ‘What does that mean?’ He said, ‘Well, three of your lymph nodes were contaminated and that means it was on its way out of your colon and into your body.’ The next place it usually takes root is in your liver. It goes from the colon into the liver, nine times out of ten that’s how colon cancer works. Once it gets into the lymph nodes, it’s in your bloodstream, and your liver filters your blood. So it’s going to be that’s the next place, because it’s trying to filter it out.”
By all accounts, this was not good news.
“What stage three means, is that your probability that you could develop cancer elsewhere in the next five years could be somewhere 50%-70% without any treatment,” Dr. Paz clarified. “It [The liver] is the most common site, but it is not the only site, because the blood goes through the liver before it goes to the rest of the body, so the liver is the most common site, but not the only one.”
“When I say we found it in the nick of time, I mean we really found it,” Sonya emphasized. “It was on its way out; Stage four was not far away. I knew, because you know your body. Honestly, the whole reason I found the cancer is because I knew my body, because I knew something wasn’t right. No matter what the doctors said, ‘Oh, it’s indigestion, it’s irritable bowel syndrome, I knew it wasn’t right and I wasn’t going to let it go, and I honestly believe that’s what saved my life, was my own persistence. Because I was so young, and because my cancer was so advanced, they automatically put me into the genetic testing.
“When they take the tumour out, they test the tumour genetically right away. Every protein that they tested before was negative, which meant that they needed to do more in-depth testing on me because how are all the tests coming out negative and here I am with stage-3 colon cancer? So they tested more, it took months, I get the results back and the results are it’s not in my genes. We still don’t know how or why I got cancer. I will probably never know because if it’s not in your genes, then you’re just a freak anomaly, is what they’ve called me. There’s ten other thirty-somethings in the City of Hope databanks that are like me. We don’t have family history, our genetics don’t have cancer in them, but yet we’ve still got a major aggressive advance cancer at an extremely young age. So we’re a bunch of medical mysteries. They talked about my genetics at a couple of conferences, because they are baffled, they are literally baffled by my case. They don’t understand it.
“One of the things that helps you get through this is knowing whatever they find out about is going to help somebody five to ten years down the road and it really does motivate you. Not necessarily motivate, but inspire you.”
Sonya Van Dam hams it up in Portugal.
For the curious, Sonya has a multi-racial background. Primarily, her mother is white, while her father’s ethnic background is Indian.
“Had my doctor, when I went in February of 2007, been responsible and done a colonoscopy at that time or even in November, it would have been stage one or two. Had he had done it when I went in for a bloody stool, it would have been what they call a polypectomy. So when they go in and they do the colonoscopy, they’ll see that there’s a ‘Polyp’ there and they’ll just remove it. Everything starts as a polyp. It’s a really small, like a skin tag. They just remove it right there, send it off to the lab and then everything’s fine because you don’t have to go through chemotherapy. Because I had the run-around and the cancer was growing, cancer grows faster in healthier bodies because it has all the things that it needs. It’s almost like a tapeworm.”
But now, Rob and Sonya were facing the biggest decision of their life. Sonya thought about talking about it with Tina but she and her other close friends were going through a lot as well.
“Tina is my best friend; 2008 was a really tough year for her,” she said. “She got married, got pregnant and had a baby all in one year. I found out I got cancer on the 5th of April; she found out she was pregnant on the 6th. So we kind of had our own stuff to deal with. She’s been there, but with the cancer, I didn’t really lean on her because she had so much on her plate already. She now has a stepson, adjusting to a new husband; she had too much, so I had some other friends that I really talked to about the process. I didn’t want to dump this all on her. I dumped it on my friend Emily in South Carolina mostly, who by the way was going through a divorce at the time and can I just tell you, I would much rather have had cancer than go through a divorce. I told Rob that too. It was kind of an ugly divorce.
“She’s like, ‘I wouldn’t trade places with you,’ and I’m like, ‘Well, I wouldn’t trade places with you!’
“Once I got staged, he tells me with Stage 3, it’s basically mandatory protocol that you go through six months of chemotherapy. I’m like, ‘Well, what am I looking at if I don’t want to take chemotherapy at stage three?
“’50-50,’ they said. They said, ‘You can walk out of here and not do chemotherapy and you have a 50-50 chance it will come back. And if it comes back, it comes back with a vengeance.’ So, I didn’t like those odds. Let me clarify that, Rob did not like those odds. He was pretty shaken up after we left that appointment, because here we are faced with this choice of: ‘We’re going to pump as much poison into your body as we can to kill the cancer but not kill you, or you can go and live your life and maybe, maybe not it will come back and kill you. So it’s literally a do-or-die situation.
“It wasn’t presented as an option that we could really just take or leave,” said Rob. “It seemed like it was very important to do this. We weren’t looking forward to it, of course, and of course, we could have refused treatment and a lot of people in her situation, her circumstances, probably would maybe not go through the chemo if they were older, if they were not in as good a shape because the chemo does take its toll on the patients. Colon cancer is something that usually people get when they’re older. It’s usually men, it’s usually older than 50, someone who eats a lot red meat. And in fact we still don’t even know how she got it, which really sucks, because if she got from let’s say the water, well damn, we’re still drinking the water.
“So that’s pretty frustrating not knowing, but knowing there was a 50-50 chance it could return because it was stage three, there was no doubt that if chemo was going to decrease the chances of it coming back, then we had to do it.”
Rob and Sonya Van Dam check out a castle in Portugal.
“There was no tension,” she insisted when queried at length. “There was absolutely no tension because for him because for him he was like, ‘You know honey, I can’t lose you; I can’t live without you. I can’t live knowing that there’s a 50-50 chance that you could be taken away from me.” When he put it exactly in those words, I was much more receptive to it. Because for me, basically it was the fear that was driving me of not wanting to do it. Fear of the unknown, fear of what was in store for me with the chemo that was my biggest fear for me. But for him to calm me down, and say ‘Look honey, we can’t do this without you.’ That put it into perspective and I was like, ‘Okay.’
“It was that simple; it really was because the compassion and love that was in his eyes. He was literally pleading with me to, ‘Do it for us. Do it for us, and we’ll get through it, and I will be there every step of the way,’ which he absolutely has been.”
“Rob’s reaction was a lot like mine, like when we were in the recovery room he also went numb. He was kind of in the same boat with me; he just didn’t hear the words coming out of the doctor’s mouth and when we talked about it later, his experiences were very similar there.
“The difference was he didn’t need the nurses to tell him; he heard it the first time where I didn’t.
“He was obviously upset, but he was very positive in that he had to convince me that it was the right thing to do. So he believed in his heart that it was the right thing to do and he just had to convince me that it was okay.
“I absolutely would not have made it without him. He was my rock.”
“I actually know people that you and I know — some people that everybody knows — that are going through this right now and keeping it private because it is a very personal matter and I can understand that,” added Rob. “Being a stickler for the truth, and believing every day our lives are tomorrow’s history. Sonya and I both feel very similar about that. That’s why if anything happens with me and people think of something they should keep hush-hush like for instance, my big bust with Sabu when I had the possession of marijuana. You’ll never ever hear me apologize about that, you’ll never hear me back away and say, ‘Oh, we can’t talk about that.’ That happened; that’s history; let’s learn from it. Sonya feels the same way and that’s one of the many reasons we are such a great team.”
“Sonya has always been very strong in facing the diagnosis and her options. She has been in tears but not overwhelmed by it,” Dr. Paz said when asked for his perspective.
“Once they understand the potential consequences and how they are to manage through the treatment, they do well. The aim is to make sure we convey the information correctly and help patients to face the treatment with dignity. All of these things take a lot of work, but we are blessed to have a team of physicians, nurses, and a hospital dedicated to this. The doctors I work with everyday not only care about the difficult aspects of the cancer patients, they really care about the psychological aspects well.
“We work with our patients.”
There was still a long way to go however. The Van Dams had decided to undergo chemotherapy, a six-month process.
RELATED LINKS